Biomedical applications of soft robotics
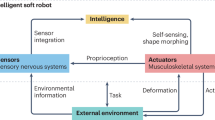
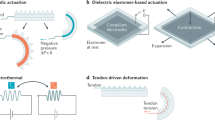
Soft robotics enables the design of soft machines and devices at different scales. The compliance and mechanical properties of soft robots make them especially interesting for medical applications. Depending on the level of interaction with humans, different levels of biocompatibility and biomimicry are required for soft materials used in robots. In this Review, we investigate soft robots for biomedical applications, including soft tools for surgery, diagnosis and drug delivery, wearable and assistive devices, prostheses, artificial organs and tissue-mimicking active simulators for training and biomechanical studies. We highlight challenges regarding durability and reliability, and examine traditional and novel soft and active materials as well as different actuation strategies. Finally, we discuss future approaches and applications in the field.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
133,45 € per year
only 11,12 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Bioinspired electronics for intelligent soft robots
Article 05 August 2024
Soft actuators for real-world applications
Article 10 November 2021

Untethered soft actuators for soft standalone robotics
Article Open access 25 April 2024
References
- Wang, L. & Iida, F. Deformation in soft-matter robotics: a categorization and quantitative characterization. IEEE Robot. Autom. Mag.22, 125–139 (2015). ArticleGoogle Scholar
- Laschi, C., Mazzolai, B. & Cianchetti, M. Soft robotics: Technologies and systems pushing the boundaries of robot abilities. Sci. Robot.1, eaah3690 (2016). ArticleGoogle Scholar
- Cianchetti, M. & Laschi, C. Pleasant to the Touch: By emulating nature, scientists hope to find innovative new uses for soft robotics in health-care technology. IEEE Pulse7, 34–37 (2016). ArticleGoogle Scholar
- McEvoy, M. A. & Correll, N. Materials that couple sensing, actuation, computation, and communication. Science347, 1261689 (2015). ArticleGoogle Scholar
- Manti, M., Cacucciolo, V. & Cianchetti, M. Stiffening in soft robotics: a review of the state of the art. IEEE Robot. Autom. Mag.23, 93–106 (2016). ArticleGoogle Scholar
- Pfeifer, R., Lungarella, M. & Iida, F. The challenges ahead for bio-inspired ‘soft’ robotics. Commun. ACM55, 76 (2012). ArticleGoogle Scholar
- Rané, A., Tan, G. Y. & Tewari, A. K. Laparo-endoscopic single-site surgery in urology: is robotics the missing link? BJU Int.104, 1041–1043 (2009). ArticleGoogle Scholar
- Vitiello, V., Lee, S.-L., Cundy, T. P. & Yang, G.-Z. Emerging robotic platforms for minimally invasive surgery. IEEE Rev. Biomed. Eng.6, 111–126 (2013). ArticleGoogle Scholar
- Vyas, L., Aquino, D., Kuo, C.-H., Dai, J. S. & Dasgupta, P. Flexible robotics. BJU Int.107, 187–189 (2011). ArticleGoogle Scholar
- Loeve, A., Breedveld, P. & Dankelman, J. Scopes too flexible…and too stiff. IEEE Pulse1, 26–41 (2010). ArticleGoogle Scholar
- Le, H. M., Do, T. N. & Phee, S. J. A survey on actuators-driven surgical robots. Sens. Actuators A Phys.247, 323–354 (2016). ArticleGoogle Scholar
- Ikuta, K., Tsukamoto, M. & Hirose, S. in Proceedings. 1988 IEEE International Conference on Robotics and Automation 427–430 (Philadelphia, PA, USA, 1988).
- Menciassi, A. et al. Shape memory alloy clamping devices of a capsule for monitoring tasks in the gastrointestinal tract. J. Micromech. Microeng.15, 2045–2055 (2005). ArticleGoogle Scholar
- Robinson, G. & Davies, J. B. C. in Proceedings 1999 IEEE International Conference on Robotics and Automation 2849–2854 (Detroit, MI, USA, 1999).
- Burgner-Kahrs, J., Caleb Rucker, D. & Choset, H. Continuum robots for medical applications: a survey. IEEE Trans. Rob.31, 1261–1280 (2015). ArticleGoogle Scholar
- Polygerinos, P. et al. Soft Robotics: Review of fluid-driven intrinsically soft devices; manufacturing, sensing, control, and applications in human-robot interaction. Adv. Eng. Mater.19, 1700016 (2017). ArticleGoogle Scholar
- Phee, L. et al. Analysis and development of locomotion devices for the gastrointestinal tract. IEEE Trans. Biomed. Eng.49, 613–616 (2002). ArticleGoogle Scholar
- Bertetto, A. M. et al. A novel fluidic bellows manipulator. J. Robot. Mechatron.16, 604–612 (2004). ArticleGoogle Scholar
- Volder, M. D. et al. Production and characterization of a hydraulic microactuator. J. Micromech. Microeng.15, S15–S21 (2005). ArticleGoogle Scholar
- Howell, L. L., Magleby, S. P. & Olsen, B. M. Handbook of Compliant Mechanisms. (John Wiley & Sons, 2013).
- De Greef, A., Lambert, P. & Delchambre, A. Towards flexible medical instruments: review of flexible fluidic actuators. Precis. Eng.33, 311–321 (2009). ArticleGoogle Scholar
- Comber, D. B., Slightam, J. E., Gervasi, V. R., Neimat, J. S. & Barth, E. J. Design, additive manufacture, and control of a pneumatic MR-compatible needle driver. IEEE Trans. Rob.32, 138–149 (2016). ArticleGoogle Scholar
- Suzumori, K. Elastic materials producing compliant robots. Rob. Auton. Syst.18, 135–140 (1996). ArticleGoogle Scholar
- Suzumori, K., Koga, A., Kondo, F. & Haneda, R. Integrated flexible microactuator systems. Robotica14, 493 (1996). ArticleGoogle Scholar
- Ranzani, T., Gerboni, G., Cianchetti, M. & Menciassi, A. A bioinspired soft manipulator for minimally invasive surgery. Bioinspir. Biomim.10, 035008 (2015). ArticleGoogle Scholar
- Arezzo, A. et al. Total mesorectal excision using a soft and flexible robotic arm: a feasibility study in cadaver models. Surg. Endosc.31, 264–273 (2016). ArticleGoogle Scholar
- Konishi, S., Kawai, F. & Cusin, P. Thin flexible end-effector using pneumatic balloon actuator. Sens. Actuators A Phys.89, 28–35 (2001). ArticleGoogle Scholar
- Noritsugu, T. et al. Development of pneumatic rotary soft actuator made of silicone rubber. J. Robot. Mechatron.13, 17–22 (2001). ArticleGoogle Scholar
- Yang, Q. et al. in IEEE Conference on Robotics, Automation and Mechatronics, 2004https://doi.org/10.1109/RAMECH.2004.1438950 (Singapore, 2004).
- Suzumori, K., Iikura, S. & Tanaka, H. in [1991] Proceedings. IEEE Micro Electro Mechanical Systems 204–209 (Nara, Japan, 1991).
- Low, J.-H., Delgado-Martinez, I. & Yeow, C.-H. Customizable soft pneumatic chamber–gripper devices for delicate surgical manipulation. J. Med. Device.8, 044504 (2014). ArticleGoogle Scholar
- Gerboni, G. et al. A novel linear elastic actuator for minimally invasive surgery: development of a surgical gripper. Smart Mater. Struct.25, 105025 (2016). ArticleGoogle Scholar
- Ranzani, T., Cianchetti, M., Gerboni, G., De Falco, I. & Menciassi, A. A. Soft modular manipulator for minimally invasive surgery: design and characterization of a single module. IEEE Trans. Rob.32, 187–200 (2016). ArticleGoogle Scholar
- Lazeroms, M. et al. A hydraulic forceps with force-feedback for use in minimally invasive surgery. Mechatronics6, 437–446 (1996). ArticleGoogle Scholar
- Gerboni, G. et al. Modular soft mechatronic manipulator for minimally invasive surgery (MIS): overall architecture and development of a fully integrated soft module. Meccanica50, 2865–2878 (2015). ArticleGoogle Scholar
- Moers, A. J. M., De Volder, M. F. L. & Reynaerts, D. Integrated high pressure microhydraulic actuation and control for surgical instruments. Biomed. Microdevices14, 699–708 (2012). ArticleGoogle Scholar
- Ikuta, K., Ichikawa, H., Suzuki, K. & Yamamoto, T. in 2003 IEEE International Conference on Robotics and Automationhttps://doi.org/10.1109/robot.2003.1241991 (Taipei, Taiwan, 2004)
- Ruzzu, A., Bade, K., Fahrenberg, J. & Maas, D. Positioning system for catheter tips based on an active microvalve system. J. Micromech. Microeng.8, 161–164 (1998). ArticleGoogle Scholar
- Sun, Y., Song, S., Liang, X. & Ren, H. A. Miniature soft robotic manipulator based on novel fabrication methods. IEEE Robot. Autom. Lett.1, 617–623 (2016). ArticleGoogle Scholar
- Gorissen, B., Vincentie, W., Al-Bender, F., Reynaerts, D. & De Volder, M. Modeling and bonding-free fabrication of flexible fluidic microactuators with a bending motion. J. Micromech. Microeng.23, 045012 (2013). ArticleGoogle Scholar
- Diodato, A. et al. Soft robotic manipulator for improving dexterity in minimally invasive surgery. Surg. Innov.25, 69–76 (2018). ArticleGoogle Scholar
- Karki, S. et al. Thin films as an emerging platform for drug delivery. Asian J. Pharm. Sci.11, 559–574 (2016). ArticleGoogle Scholar
- Borodkin, S. & Tucker, F. E. Drug release from hydroxypropyl cellulose-polyvinyl acetate films. J. Pharm. Sci.63, 1359–1364 (1974). ArticleGoogle Scholar
- Fusco, S. et al. An integrated microrobotic platform for on-demand, targeted therapeutic interventions. Adv. Mater.26, 952–957 (2014). ArticleGoogle Scholar
- Breger, J. C. et al. Self-folding thermo-magnetically responsive soft microgrippers. ACS Appl. Mater. Interfaces7, 3398–3405 (2015). ArticleGoogle Scholar
- Ricotti, L. et al. Biohybrid actuators for robotics: A review of devices actuated by living cells. Sci. Robot.2, eaaq0495 (2017). ArticleGoogle Scholar
- Tefertiller, C., Pharo, B., Evans, N. & Winchester, P. Efficacy of rehabilitation robotics for walking training in neurological disorders: a review. J. Rehabil. Res. Dev.48, 387–416 (2011). ArticleGoogle Scholar
- Herr, H. M. & Kornbluh, R. D. in Proc. SPIE 5385, Smart Structures and Materials 2004: Electroactive Polymer Actuators and Devices (EAPAD)https://doi.org/10.1117/12.544510 (San Diego, CA, USA, 2004).
- Gordon, K. E., Sawicki, G. S. & Ferris, D. P. Mechanical performance of artificial pneumatic muscles to power an ankle–foot orthosis. J. Biomech.39, 1832–1841 (2006). ArticleGoogle Scholar
- do Nascimento, B. G., Vimieiro, C. B. S., Nagem, D. A. P. & Pinotti, M. Hip orthosis powered by pneumatic artificial muscle: voluntary activation in absence of myoelectrical signal. Artif. Organs32, 317–322 (2008). ArticleGoogle Scholar
- Kawamura, T., Takanaka, K., Nakamura, T. & Osumi, H. in 2013 IEEE 13th International Conference on Rehabilitation Robotics (ICORR)https://doi.org/10.1109/ICORR.2013.6650350 (Seattle, WA, USA, 2013).
- Pittaccio, S. et al. SHADE: a shape-memory-activated device promoting ankle dorsiflexion. J. Mater. Eng. Perform.18, 824–830 (2009). ArticleGoogle Scholar
- Pittaccio, S. & Viscuso, S. An EMG-controlled SMA device for the rehabilitation of the ankle joint in post-acute stroke. J. Mater. Eng. Perform.20, 666–670 (2011). ArticleGoogle Scholar
- Stirling, L. et al. Applicability of shape memory alloy wire for an active, soft orthotic. J. Mater. Eng. Perform.20, 658–662 (2011). ArticleGoogle Scholar
- Park, Y.-L. et al. Design and control of a bio-inspired soft wearable robotic device for ankle–foot rehabilitation. Bioinspir. Biomim.9, 016007 (2014). ArticleGoogle Scholar
- Wehner, M. et al. in 2013 IEEE International Conference on Robotics and Automation 3362–3369 (Karlsruhe, Germany, 2013).
- Asbeck, A. T., De Rossi, S. M. M., Holt, K. G. & Walsh, C. J. A biologically inspired soft exosuit for walking assistance. Int. J. Rob. Res.34, 744–762 (2015). ArticleGoogle Scholar
- Awad, L. N. et al. A soft robotic exosuit improves walking in patients after stroke. Sci. Transl Med.9, eaai9084 (2017). ArticleGoogle Scholar
- Mengüç, Y. et al. Wearable soft sensing suit for human gait measurement. Int. J. Rob. Res.33, 1748–1764 (2014). ArticleGoogle Scholar
- Tsagarakis, N. G. & Caldwell, D. G. Development and control of a ‘soft-actuated’ exoskeleton for use in physiotherapy and training. Autonom. Robots15, 21–33 (2003). ArticleGoogle Scholar
- Villoslada, A., Flores, A., Copaci, D., Blanco, D. & Moreno, L. High-displacement flexible shape memory alloy actuator for soft wearable robots. Rob. Auton. Syst.73, 91–101 (2015). ArticleGoogle Scholar
- Copaci, D., Cano, E., Moreno, L. & Blanco, D. New design of a soft robotics wearable elbow exoskeleton based on shape memory alloy wire actuators. Appl. Bion. Biomech.2017, 1605101 (2017). Google Scholar
- Galiana, I., Hammond, F. L., Howe, R. D. & Popovic, M. B. in 2012 IEEE/RSJ International Conference on Intelligent Robots and Systems 317–322 (Vilamoura, Portugal, 2012).
- Natividad, R. F. & Yeow, C. H. in 2016 6th IEEE International Conference on Biomedical Robotics and Biomechatronics (BioRob) 989–993 (Singapore, 2016).
- Kim, D. H., Heo, S.-H. & Park, H.-S. in 2017 International Conference on Rehabilitation Robotics (ICORR) 1326–1330 (London, UK, 2017).
- Maeder-York, P. et al. Biologically inspired soft robot for thumb rehabilitation. J. Med. Device.8, 020934 (2014). ArticleGoogle Scholar
- Carpi, F., Mannini, A. & De Rossi, D. Proc. SPIE 6927, Electroactive Polymer Actuators and Devices (EAPAD) 2008https://doi.org/10.1117/12.774644 (San Diego, CA, USA, 2008).
- Delph, M. A. et al. in 2013 IEEE 13th International Conference on Rehabilitation Robotics (ICORR)https://doi.org/10.1109/ICORR.2013.6650426 (Seattle, WA, USA, 2013).
- In, H., Kang, B. B., Sin, M. & Cho, K.-J. Exo-Glove: a wearable robot for the hand with a soft tendon routing system. IEEE Robot. Autom. Mag.22, 97–105 (2015). ArticleGoogle Scholar
- Kang, B. B. et al. in 2016 IEEE International Conference on Robotics and Automation (ICRA) 3750–3755 (Stockholm, Sweden, 2016).
- Connelly, L. et al. A pneumatic glove and immersive virtual reality environment for hand rehabilitative training after stroke. IEEE Trans. Neural Syst. Rehabil. Eng.18, 551–559 (2010). ArticleGoogle Scholar
- Guo, S. et al. in 2015 IEEE International Conference on Mechatronics and Automation (ICMA) 2197–2202 (Beijing, China, 2015).
- Polygerinos, P., Wang, Z., Galloway, K. C., Wood, R. J. & Walsh, C. J. Soft robotic glove for combined assistance and at-home rehabilitation. Robot. Auton. Syst.73, 135–143 (2015). ArticleGoogle Scholar
- Ilievski, F., Mazzeo, A. D., Shepherd, R. F., Chen, X. & Whitesides, G. M. Soft robotics for chemists. Angew. Chem. Int. Ed.50, 1890–1895 (2011). ArticleGoogle Scholar
- Yeo, J. C. et al. Flexible and stretchable strain sensing actuator for wearable soft robotic applications. Adv. Mater. Technol.1, 1600018 (2016). ArticleGoogle Scholar
- Yap, H. K., Lim, J. H., Nasrallah, F. & Yeow, C.-H. Design and preliminary feasibility study of a soft robotic glove for hand function assistance in stroke survivors. Front. Neurosci.11, 547 (2017). ArticleGoogle Scholar
- Manto, M. et al. Dynamically responsive intervention for tremor suppression. IEEE Eng. Med. Biol. Mag.22, 120–132 (2003). ArticleGoogle Scholar
- Ansari, Y. et al. Towards the development of a soft manipulator as an assistive robot for personal care of elderly people. Int. J. Adv. Rob. Syst.14, 172988141668713 (2017). ArticleGoogle Scholar
- Pfeifer, R. & Bongard, J. How the Body Shapes the Way We Think: A New View of Intelligence. (MIT Press, 2006).
- Deimel, R. & Brock, O. A novel type of compliant and underactuated robotic hand for dexterous grasping. Int. J. Rob. Res.35, 161–185 (2015). ArticleGoogle Scholar
- Galloway, K. C. et al. Soft robotic grippers for biological sampling on deep reefs. Soft Robot.3, 23–33 (2016). ArticleGoogle Scholar
- Mutlu, R., Alici, G., in het Panhuis, P. & Spinks, G. M. 3D printed flexure hinges for soft monolithic prosthetic fingers. Soft Robot.3, 120–133 (2016). ArticleGoogle Scholar
- Thompson-Bean, E., Das, R. & McDaid, A. Methodology for designing and manufacturing complex biologically inspired soft robotic fluidic actuators: prosthetic hand case study. Bioinspir. Biomim.11, 066005 (2016). ArticleGoogle Scholar
- Cheng, N. et al. Prosthetic jamming terminal device: a case study of untethered soft robotics. Soft Robot.3, 205–212 (2016). ArticleGoogle Scholar
- Ogawa, A., Obinata, G., Hase, K., Dutta, A. & Nakagawa, M. in 2008 30th Annual International Conference of the IEEE Engineering in Medicine and Biology Society 330–333 (Vancouver, BC, Canada, 2008).
- Paterno, L., Ibrahimi, M., Gruppioni, E., Menciassi, A. & Ricotti, L. Sockets for limb prostheses: a review of existing technologies and open challenges. IEEE Trans. Biomed. Engineer. https://doi.org/10.1109/TBME.2017.2775100 (2018).
- Roche, E. T. et al. A bioinspired soft actuated material. Adv. Mater.26, 1200–1206 (2014). ArticleGoogle Scholar
- Roche, E. T. et al. Soft robotic sleeve supports heart function. Sci. Transl Med.9, eaaf3925 (2017). ArticleGoogle Scholar
- Payne, C. J. et al. An implantable extracardiac soft robotic device for the failing heart: mechanical coupling and synchronization. Soft Robot.4, 241–250 (2017). Google Scholar
- Horvath, M. A. et al. An intracardiac soft robotic device for augmentation of blood ejection from the failing right ventricle. Ann. Biomed. Eng.45, 2222–2233 (2017). ArticleGoogle Scholar
- Cohrs, N. H. et al. A soft total artificial heart-first concept evaluation on a hybrid mock circulation. Artif. Organs41, 948–958 (2017). ArticleGoogle Scholar
- Schumacher, C. M., Loepfe, M., Fuhrer, R., Grass, R. N. & Stark, W. J. 3D printed lost-wax casted soft silicone monoblocks enable heart-inspired pumping by internal combustion. RSC Adv.4, 16039–16042 (2014). ArticleGoogle Scholar
- Mac Murray, B. C. et al. Poroelastic foams for simple fabrication of complex soft robots. Adv. Mater.27, 6334–6340 (2015). ArticleGoogle Scholar
- Irwin, D. E., Kopp, Z. S., Agatep, B., Milsom, I. & Abrams, P. Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence and bladder outlet obstruction. BJU Int.108, 1132–1138 (2011). ArticleGoogle Scholar
- Chonan, S. et al. Development of an artificial urethral valve using SMA actuators. Smart Mater. Struct.6, 410–414 (1997). ArticleGoogle Scholar
- Weiss, F. M., Deyhle, H., Kovacs, G. & Müller, B. in Proc. SPIE 8340, Electroactive Polymer Actuators and Devices (EAPAD) 2012https://doi.org/10.1117/12.914649 (San Diego, CA, USA, 2012).
- Hached, S. et al. Novel, wirelessly controlled, and adaptive artificial urinary sphincter. IEEE/ASME Trans. Mechatron.20, 3040–3052 (2015). ArticleGoogle Scholar
- Lamraoui, H. et al. Development of a novel artificial urinary sphincter: a versatile automated device. IEEE/ASME Trans. Mechatron.15, 916–924 (2010). Google Scholar
- Baldoli, I. et al. A novel simulator for mechanical ventilation in newborns: MEchatronic REspiratory System SImulator for Neonatal Applications. Proc. Inst. Mech. Eng. H229, 581–591 (2015). ArticleGoogle Scholar
- Kim, S., Kim, P., Park, C.-Y. & Choi, S.-B. A new tactile device using magneto-rheological sponge cells for medical applications: experimental investigation. Sens. Actuators A Phys.239, 61–69 (2016). ArticleGoogle Scholar
- Someya, Y. et al. in 2016 International Symposium on Micro-NanoMechatronics and Human Science (MHS)https://doi.org/10.1109/MHS.2016.7824208 (Nagoya, Japan, 2016).
- Manti, M., Cianchetti, M., Nacci, A., Ursino, F. & Laschi, C. in 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC) 3623–3626 (2015).
- Zhu, M., Xu, W. & Cheng, L. K. Esophageal peristaltic control of a soft-bodied swallowing robot by the central pattern generator. IEEE/ASME Trans. Mechatron.22, 91–98 (2017). ArticleGoogle Scholar
- Lu, X., Xu, W. & Li, X. A. Soft robotic tongue — mechatronic design and surface reconstruction. IEEE/ASME Trans. Mechatron.22, 2102–2110 (2017). ArticleGoogle Scholar
- Wehner, M. et al. Pneumatic energy sources for autonomous and wearable soft robotics. Soft Robot.1, 263–274 (2014). ArticleGoogle Scholar
- Roseman, J. M. et al. Hybrid integrated biological–solid-state system powered with adenosine triphosphate. Nat. Commun.6, 10070 (2015). ArticleGoogle Scholar
- Menciassi, A. Swell findings in hydrogels. N. Engl. J. Med.378, 864–865 (2018). ArticleGoogle Scholar
Acknowledgements
The authors acknowledge support from the European Commission through the Hybrid Heart (#767195) and I-SUPPORT (#643666) projects.